Lower Leg Injury Resource Center
Below Knee Amputation
Surgery, Recovery and Maintaining Mobility
There are 1.8 million people living with amputations, and between 30,000 and 40,000 amputations performed on an annual basis in the United States [1]. Below knee amputations are the most common amputation surgery and comprise about 23 percent of lower limb amputation surgeries. The majority of below knee amputations are performed on individuals 65 and older.
Any form of amputation is a life-changing event, but it’s important to remember that amputations are viewed as a reconstruction surgery with the goal of returning the patient to a normal life. Advances in medical technology and prosthetics have helped many patients return to a relatively pain-free and active lifestyle after amputation surgery.
Your Guide To BKA Recovery
Causes of Below Knee Amputation
Tips for Successful BK Amputation
Is Below Knee Amputation Right for Me?
Staying Mobile Prior to BK Amputation
What to Expect From Below Knee Amputation Surgery
Below Knee Amputation Recovery
Complications From Below Knee Amputation
Living as a Below Knee Amputee
Support Organizations for Below Knee Amputees
I
CAUSES OF BELOW KNEE AMPUTATIONS
Below knee amputation surgery is generally performed if a person’s lower extremity or foot has been severely injured or if he or she suffers from chronic and sever pain in the foot or lower extremity. Causes are generally related to the following:
- Trauma – A severe injury resulting from an event such as a vehicle accident or serious burn that causes severe fractures and/or nerve injuries.
- Diabetes – People who suffer from diabetes may experience poor circulation because their arteries. This is known as peripheral vascular disease (PVD). In this case, poor circulation does not allow the impacted extremities to obtain sufficient nutrients and oxygen. The affected tissue begins to deteriorate, which can lead to amputation. PVD is the leading cause of below knee amputations.
- Cancer – Untreatable tumors in the bone or muscle of a lower limb may lead to below knee amputation.
- Infections – If infections are untreatable with antibiotics or other medical remedies, removal of the lower limb may be required.
- Neuroma – Thickening of nerve tissue is called Neuroma, a condition that can cause severe pain. Neuroma most often affects feet.
- Congenital Limb Deficiency – A common cause of below knee amputation among small children, Congenital Limb Deficiency takes place when a limb does not form completely.
- Complex Regional Pain Syndrome (CRPS) – A chronic pain condition that usually affects the extremities, CRPS is typically caused by an injury or trauma. CRPS is a complicated condition that’s believed to be caused by damage to the peripheral or central nervous system.

While there are many additional reasons a person may choose below knee amputation, those listed above are most common [2].
Below knee amputation surgery is a serious undertaking aimed at resolving complicated or life-threatening issues in the foot or other parts of the leg below the knee. Any decision to amputate involves multiple factors and should include many discussions between the patient and their team of doctors.
I
TIPS FOR SUCCESSFUL BK AMPUTATION
Below knee amputation surgery is a means to improve the quality of life for many patients. There are a number of actions you can take to prepare for the surgery and facilitate your transition to an independent and, hopefully, pain-free lifestyle.
Know what to expect
Talk to your medical care team about how to prepare for surgery and what to expect from rehabilitation. Consult your primary care physician, orthopedic surgeon, prosthetist (a specialist in the design and fit of prosthetic limbs), physical therapist and rehabilitation doctor. You may also want to discuss the surgery with a psychologist, psychiatrist, social worker or another person who has already undergone below knee amputation.
Seek out a below knee amputee who is similar in age to learn what they did to make their surgery and rehabilitation successful. Find and get involved with support groups to help answer questions about the physical and psychological effects of amputation and tips about how to return to your ideal lifestyle.
Familiarize yourself with the transition to a prosthetic and seek out methods to ease that transition. (A list of support and peer groups is included at the end of this article.)
Also, begin to think about changes you’ll need to make at home. If you’ll be confined to a wheelchair for a period of time you might need to install ramps that go around or over stairs. Think about methods that will help you transition to an independent lifestyle following surgery. You may want to reposition furniture, kitchen items and other frequently-used household items to make them more accessible.
Get involved with the BKA community (blogs, YouTube, Facebook pages and support groups), and learn tips and tricks that will make your transition following surgery more comfortable.
Stay strong and healthy
Below knee amputees use approximately 25 percent more energy to walk following a BTK amputation [3], so it’s extremely important to maintain or increase your strength and overall fitness before surgery. Many doctors will prescribe exercises to maintain muscle conditioning in the upper leg and improve strength and flexibility in the hip and knee. Straight leg raises and knee extension exercises should be performed regularly before surgery.
Some below knee amputees have said learning to walk with a walker, crutches, knee scooter or a device like iWALK hands-free crutch helped them tremendously following surgery. Learning to balance while not bearing weight on one leg can be challenging, and it may take time to adjust.
Advances in medical device technology, such as with the iWALK hands-free crutch, have enabled many BKA patients to learn to walk with a prosthetic even before amputation surgery and have eased the transition to life with a prosthetic foot or prosthetic leg. Using this technology not only helps patients maintain muscle strength before surgery, but has also shown to smooth the transition to using a prosthetic leg.

Maintaining a healthy diet and proper nutrition before surgery is also important. Your body needs nutrients to maintain muscle mass and heal properly. Exercise is important, but a healthy diet can eliminate weight gain and prepare your body for a quick recovery and successful rehabilitation.
Quit Smoking
Smoking is bad for everyone, but it is especially bad for someone planning to undergo major surgery. Smoking not only causes heart and lung disease, but it can lead to a number of other complications that include compromised healing in tissue and bone, increased pain and arthritis [4].
I
IS BKA SURGERY RIGHT FOR ME?
While those suffering from severe pain or a traumatic injury in their lower leg may opt for below knee amputation surgery, there are some who don’t qualify or face challenges [5] for one or more of the following reasons:
- Inadequate blood flow – Good blood flow contributes significantly to the body’s natural healing processes. In order to heal, tissue and bone need proper nutrients and oxygen, which are delivered via the bloodstream. If you have a history of poor circulation, have a proper evaluation before any surgery.
- Spreading infection or cancer – If you are contemplating below knee amputation because of infection or tumors, it’s important to know the extent of the issue. Infections or tumors found above the knee may require a more extensive amputation.
- Muscle loss or scar tissue – Muscle loss or scar tissue can inhibit the body’s ability to heal. Below knee amputees must have sufficient skin and muscle for the wound to heal properly and to use a prosthetic.
- Inadequate knee function – Limited knee function or significant knee pain may inhibit your ability to use a prosthetic following BKA surgery.
I
STAYING MOBILE PRIOR TO BK AMPUTATION
Some people contemplating below knee amputation may choose to wait for surgery in an attempt to salvage their foot or lower leg. In most cases, this means using crutches, knee scooter, wheelchair or the iWALK hands-free crutch to maintain mobility.
Crutches, knee scooters and wheelchairs can get the job done, but the iWALK has several key advantages. First, the iWALK is the only of the aforementioned devices that doesn’t require use of your hands, which makes tasks as simple as carrying a bag of groceries a breeze.
Second, studies show that using the iWALK boosts blood flow and reduces muscle atrophy, both qualities that may accelerate healing and increase the odds of limb salvage.
Finally, the iWALK can serve as a prosthetic “training wheel” that can prepare a prospective amputee for adaptation to a permanent prosthetic leg. Learning to use the iWALK can show a person contemplating below knee amputation that life after BKA surgery is completely manageable..
I
WHAT TO EXPECT FROM BELOW KNEE AMPUTATION SURGERY
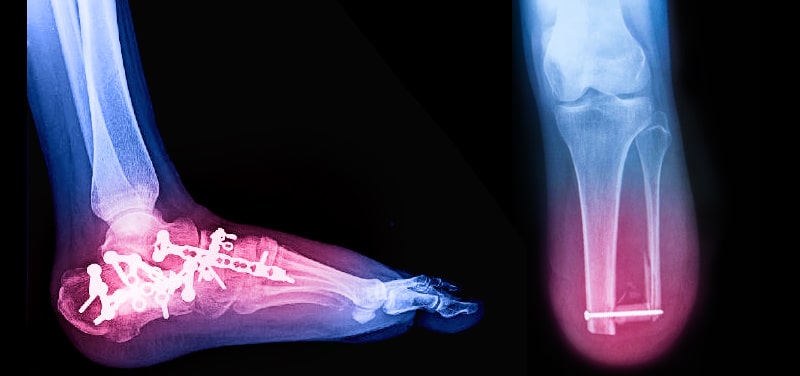
Below knee amputation is performed to remove crushed or severely fractured bone, or diseased tissue. Uneven or rough bone will be smoothed, blood vessels and nerves sealed, and muscles cut and shaped in order to prepare the remaining limb for a prosthesis.
The extent of the amputation will depend on the location of damaged tissue or bone, and, in general, there is no advantage to a longer residual limb. In fact, a longer residual limb can require use of a “low profile” prosthetic that may not work as well as a longer prosthetic. Your surgeon will attempt to leave several inches of bone below the knee in order to properly fit an artificial leg and allow for the improbable chance that a revision surgery is necessary.
Below knee amputation surgery generally lasts between two and three hours [6]. An anesthesiologist will put the patient to sleep with a nerve block and sedative or spinal anesthetic. An incision is made below the level of amputation, and the skin and calf muscles are cut away in a manner that leaves a flap or flaps that will eventually fold over the residual bone.

After leg bones are cut with a surgical saw, the flap or flaps will cover the bone and be held in place with stitches or staples on the shin side of the leg. The residual calf muscle and skin provide protection to the newly formed stump.
Hospital stays for below knee amputees range from one night to two weeks. The total amount of time depends on a patient’s overall health and how quickly they are able to gain mobility. In general, a patient may be discharged once they are able to move with crutches or a walker, or if they have help at home.

I
BELOW KNEE AMPUTATION RECOVERY
Recovery from below knee amputation is different for each patient and is highly dependent on a person’s age and overall health.
What to expect immediately following BKA surgery
In general, the incision from BKA surgery will heal over a period of two to eight weeks. During the first few days, a physical therapist will help the patient perform basic exercises and functions. These will include gentle stretching and range of motion exercises, as well as learning how to roll in bed, sit on the side of the bed, and move safely to a chair. The therapist will also teach a recent amputee to prevent contracture, a muscle tightening and deformity that can result from knees being bent too much or too long.
Protecting the limb and incision after surgery is paramount. One small bump can open the incision and delay recovery, and possibly create the need for additional surgeries.
When will I be able to walk again after BK amputation?
People heal at different paces, so it’s important to adhere to your doctor’s instructions. It’s also important to note that your incision will need to heal completely before you’re able to walk using a prosthetic leg. However, below knee amputation patients are usually able to walk with crutches soon after surgery.
Many below knee amputee patients are able to use the iWALK hands-free crutch two or more weeks after surgery. This enables them to use both legs instead of relying on crutches or a wheelchair. Unassisted walking using the iWALK facilitates independent living and is, in and of itself, a form of exercise that reduces muscle atrophy while promoting healthy blood flow and faster healing.
Swelling is a very important factor in the healing process, and all swelling must subside before a permanent artificial leg can be fitted. Swelling can take months to subside, so it’s important to be patient and find ways to get around like crutches, a knee scooter, wheelchair, or hands-free crutch like the iWALK. It’s also important to adhere to a strict exercise and stretching regiment. Maintaining strength and flexibility in your muscles, hips and knees will ease your transition to a permanent prosthesis.
There’s a learning curve associated with using an artificial leg, and patients should be prepared to learn to walk with the new limb. Parallel bars are commonly used at first, then walkers or canes to help with the transition to walking with an artificial leg.
Learning to walk again is only one part of your transition to life as an amputee. You’ll also learn to care for your residual limb. Massage and application of ointment is sometimes necessary. You should consult your prosthetist to determine the best method of care for both your residual limb and artificial limb.

I
COMPLICATIONS FROM BELOW KNEE AMPUTATION
Complications can arise from any surgery, but there are specific complications that can develop after foot or other below knee amputation surgeries [7].
Phantom limb pain – When an amputee can still feel pain in the amputated limb it’s called phantom limb pain. While the limb is no longer there, nerve endings continue to send signals to the brain, and they’re interpreted as stinging, cramping, burning or other uncomfortable sensations. These symptoms generally subside over a period of about six months.
Atrophy – Loss of muscle strength and mass, called atrophy, can occur because the affected limb is not used as much or at all. Atrophy occurs immediately, and muscles can deteriorate at a rate of 1 to 2 percent per day.
Bone spur overgrowth – Sometimes an undesired bone formation will take shape at the end of the residual limb, and it may affect a person’s ability to wear a prosthesis. Implants can be used to inhibit bone spur formation.
Contracture – Muscle tightness that limits motion in the joints is called contracture. Most common in the knee or hip, contracture is caused by lack of movement in the affected joint. It is very important to maintain proper joint posture and range of motion to avoid contracture.
Psychological effects – The emotional challenges of losing a limb can include fear, depression, grief and more. It’s vital for recent amputees to seek counseling and support from a psychologist or social worker, as well as the amputee community. Remember, amputations are performed to help people return to an active and independent lifestyle.
I
LIVING AS A BELOW KNEE AMPUTEE
Amputation is a physical challenge, but it’s a big emotional challenge as well. It’s not uncommon for recent amputees to be overcome with feelings of grief. Recent amputees should give themselves time to adjust to a new body image. Emotional support is just as important as physical therapy, so turning to counselors, social workers, and other below knee amputees to discuss your new lifestyle is integral to the process.
Lifestyle Following BK Amputation
Over time, your physical activity will increase, and you’ll gain independence and confidence. You’ll become more comfortable walking with your artificial limb, especially navigating stairs and uneven terrain. You’ll first learn to maneuver within your living space, but those skills will quickly translate to the world outside your home’s walls. Taking a shower will require new skills, and you may find that a stool, shower chair or hands-free crutch like the iWALK is necessary.
Crawling may be necessary when using the bathroom at night or other times when you aren’t wearing your prosthetic or using crutches. As time goes on, you’ll learn what works for you and that living as an amputee does not necessarily mean your pre-amputation lifestyle has been compromised [8].

I
YOUR BELOW KNEE PROSTHESIS
Your prosthesis will return the mobility you lost due to pain before your surgery and during the recovery period immediately following surgery. While this is a very exciting phase for many amputees, it’s important to prepare to use a prosthesis and learn to care for it. This will allow you to receive maximum benefit from your artificial limb.
Maintain or Build Strength – Work as hard as you can to maintain muscle strength before surgery and as soon as the doctor allows after surgery. Walking with a prosthesis takes more energy than walking on your feet, so it’s important to keep your leg muscles strong and healthy. Performing conditioning exercises before and after surgery is often recommended and will help you gain mobility quickly. Maintaining muscle mass by using the iWALK hands-free crutch can be a significant benefit during the period after amputation and before you’ve been fitted with a below knee prosthesis.
Below Knee Prosthesis Care – Carefully follow washing instructions on any parts of your prosthesis that come into contact with your skin including liners, socks, and the inside of the socket. Be sure to allow ample time for washed parts to dry to avoid fungal growth that could lead to infection or abrasion.
Below Knee Prosthesis Tips – Know how to fit your socket correctly. If it’ too big or small, see your prosthetist immediately. Keep a bag handy that includes anything you may need in an emergency including socks, bandages and ointment. The fit of your prosthesis changes throughout the day, so keep extra pairs of socks around and put them on when needed.
Maintain Comfort With Your Prosthesis
Maintaining comfort is one of the most important parts of wearing a below knee prosthesis. At a basic level, comfort is achieved by good pressure distribution and managing friction that occurs between the prosthesis and your limb. There are also accessories that will help:
Suspension Products – Sleeves are used to hold the prosthesis firmly to your limb and keep it from slipping or turning during all phases of the walking motion. They are generally made from neoprene or silicone gel and come in a variety of sizes.
Prosthetic Socks and Sheaths – Prosthetic sheaths, liners and socks are the materials in contact with your residual limb. A prosthetic sheath helps ease friction between the skin and sock. The prosthetic sock is used to help maintain a comfortable and even fit in the event that the volume of the residual limb changes. This is accomplished either by changing to a thicker sock or wearing more than one at a time.
Caring for your Residual Limb – Wash your limb with soap and water each day (more often if you perspire heavily) and allow it to dry completely. Check your limb for any redness that doesn’t dissipate within a few minutes after removing the prosthesis. Also check for skin breakdown. You may need to use a mirror if you can’t see the end of your limb. If you have skin breakdown, stop using your prosthesis immediately, and contact your prosthetist in order to arrange for an adjustment.
I
PERMANENT PROSTHETIC ALTERNATIVES
There are times when you may not be able to or won’t want to wear your below knee prosthesis. This may occur at the end of the day when you’re simply relaxing in your home, taking a shower, or are doing something that may damage or stain your prosthesis. Options are similar to those you considered prior to BK amputation surgery.
Wheelchair
Some amputees use wheelchairs in their homes. This is easier if you have a single story, large home. Those with small or minimal stairs may decide it’s worthwhile to retrofit their home with ramps.

Traditional Crutches
Crutches are often used by below knee amputees to navigate their homes when they’re not using a prosthesis. While crutches enable mobility, they require use of the hands and arms and can be awkward and painful to use.

Knee Scooters or Knee Walkers
A knee scooter allows an amputee to rest the bent residual limb on a soft pad. The device can then be rolled on a flat surface using handlebars to steer and your other leg to push. This enables mobility throughout the house. The drawback to a knee scooter is that it requires use of your hands and can be cumbersome in small spaces.

iWALK Hands-Free Crutch
The iWALK is the only hands-free mobility device. What started as a crutch alternative for people with foot, ankle and other lower limb ailments has become a game-changer for below knee amputees. It’s easy to use, quick to put on, and allows the amputee to walk as if they were wearing their permanent prosthesis. Many amputees us the iWALK crutch at the end of the day when they’re tired of wearing their prosthesis, in the middle of the night to use the restroom, in the shower, and when their permanent prosthesis is damaged or being fitted. To learn more about the iWALK crutch, click here.

I
BK AMPUTATION SUMMARY
While below knee amputation surgery is a life-changing event, the outcome is usually quite positive. Many people who opt for below knee amputation were living in tremendous pain prior to surgery. The inherent benefits of removing a painful foot or partial limb are realized very soon after surgery. In addition, many below knee amputees have found they are able to live an independent, comfortable, and active lifestyle after surgery. Advances in surgical procedures, prosthetics, and temporary or alternative prostheses such as the iWALK hands-free crutch have helped below knee amputation patients fight pain, recover from serious injuries, and live full and active lives.
I
SUPPORT ORGANIZATIONS FOR BELOW KNEE AMPUTEES
- Local hospitals should have an organization for amputees or will know of support groups in the immediate area.
- Search Google or YouTube to find an amputee group or Google Blog by an amputee, such as AmputeeOT.
- Search Facebook for additional organizations, groups and resources for amputees.
- The Amputee Coalition’s mission is to reach out to and empower people affected by limb loss to achieve their full potential through education, support and advocacy, and to promote limb loss prevention.
- The Amputee Connection of Redlands, California is a support group for those who have suffered limb loss, or who will be having the surgery in the near future.
- The Dallas Amputee Network has programs and resource information about new materials and techniques in prosthetics, and promotes physical fitness and social interaction for a healthier lifestyle, with “Un-limb-ited Possibilities.”
- San Antonio Amputee Foundation is home to an active community and many online resources for the amputee community.
- COP Amputee Association is a support group made up of individuals who have all suffered limb loss, their families and others affected by limb loss.
- New England Amputee Association is an organization with monthly meetings, numerous events, scholarships and resources for the amputee community.
- American Orthopaedic Foot and Ankle Society is a thorough resource for a myriad conditions and procedures related to the foot and ankle, including below knee amputation.
The information above is intended for informational purposes only and is not intended to prevent, treat, or diagnose any illness or disease. We aim to provide the highest quality information, so if you have any questions on the information above, we welcome your feedback!
I
RESOURCES
- Janos P Ertl, MD. Lower Extremity Amputations. Medscape. 21 April 2021. https://emedicine.medscape.com/article/1232102-overview
- Amputation. John’s Hopkins Medicine. Accessed 21 July 2021. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/amputation
- Kahle, J. T., Highsmith, M. J., Schaepper, H., Johannesson, A., Orendurff, M. S., & Kaufman, K. (2016). Predicting Walking Ability Following Lower Limb Amputation: An Updated Systematic Literature Review. Technology and innovation, 18(2-3), 125–137. https://doi.org/10.21300/18.2-3.2016.125
- Smoking. American Society of Anesthesiologists. Accessed 21 July 2021. https://www.asahq.org/whensecondscount/preparing-for-surgery/risks/smoking/
- Brown, B. J., & Attinger, C. E. (2013). The Below-Knee Amputation: To Amputate or Palliate?. Advances in wound care, 2(1), 30–35. https://doi.org/10.1089/wound.2011.0317
- Below-the-Knee Amputation. Beth Israel Lahey Health Winchester Hospital. Accessed 21 July 2021. https://www.winchesterhospital.org/health-library/article?id=529356
- Complications Post Amputation. Physiopedia. Accessed 21 July 2021. https://www.physio-pedia.com/Complications_Post_Amputation
- Neal Conan, host, Talk of the Nation. Learning to Live as an Amputee. NPR. 22 April 2013. https://www.npr.org/2013/04/22/178436361/learning-to-live-as-an-amputee
- Mary Ann Dunkin. Amputation Overview. WebMD. 5 February 2020. https://www.webmd.com/a-to-z-guides/definition-amputation